Home > Hiking hints > Health & safety > Ticks
Tick, toc, tick ...
Tick bites
African tick bite fever
There are various types of ticks and tick-borne diseases. Many articles in South African magazines are copied from overseas published medical books and do not reflect the disease that we, as hikers, are specifically exposed to in South Africa. They often refer to among others e.g. Rocky Mountain Spotted Fever, Lymes disease, Mediterranean Spotted fever.
This article refers to the African Tick Bite Fever, (ATBF) which is what we commonly get in Sub Saharan Africa.
What causes tick bite fever?
ATBF is caused by a Rickettsial infection transmitted by ticks.
These organisms are relatively small - about 2/1000ths of a millimetre long- and are only able to survive inside cells. They are found in certain wild and domestic animals such as cattle and Game, and ticks acquire the organisms when they feed on these animals. There are thought to be two main species that cause the infection in South Africa - Rickettsia conorii and Rickettsia africae. The one we normally get is Rickettsia africae.
When the tick bites a human, the Rickettsia is transmitted in their saliva. The Rickettsia can also be transmitted from ticks to their offspring when still in the egg stage i.e. the Rickettsiae infect the eggs of the tick and thus infect the offspring.
How do we get ATBF?
Obviously from ticks. The Rickettsiae are transmitted in the saliva of an infected tick when it bites humans. Alternatively, if the tick is crushed on your skin, the Rickettsiae may be able to enter through a small abrasion.
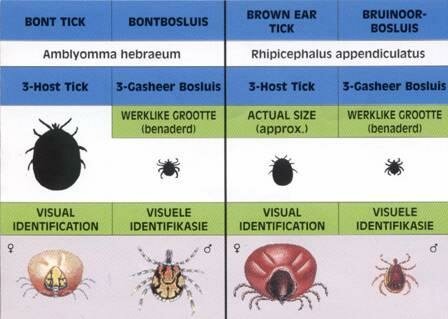
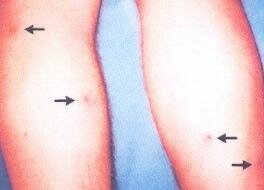
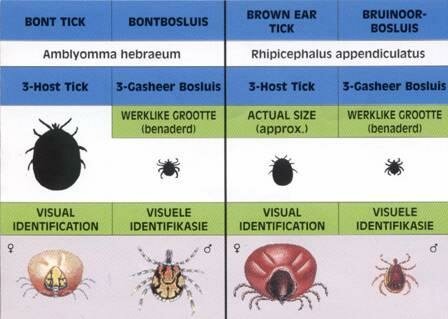
The ticks that are able to harbour the organism belong to either the Amblyomma or the Rhipicephalus family of ticks. The Amblyomma ticks actively seek out humans to feed on, while Rhipicephalus ticks tend to lie in wait on grass, and will bite you if you walk past.
These ticks have various stages of life cycles from egg to adult. The intermediate stage is what we know as a “Pepper Tick”. The different types of “Pepper Ticks” are indistinguishable to the naked eye. For those that haven’t seen them, they look like very small beauty spots on your body, only these ones have legs!! I always tell fellow hikers “if you see a beauty spot on you that is kicking,- kill it!”
The male and female adult looks very different, especially when the female is engorged with blood. When she is not engorged, she is similar to the males. See illustrations below.
Both the Pepper Tick and the adults are able to transmit the disease.
The ticks can have a one, two or three host life cycle. Amblyomma and Rhipicephalus have three hosts which could include livestock, game, hares, birds etc.
 |
 |
Symptoms and signs of tick bite fever
If you get bitten by an infected tick, the incubation period (the period between being infected and displaying symptoms) is about five to seven days.
Symptoms can vary, depending partly on the organism involved (R. africae tends to produce somewhat milder symptoms than R. conorii). Your age and underlying health may also influence the severity of the infection.
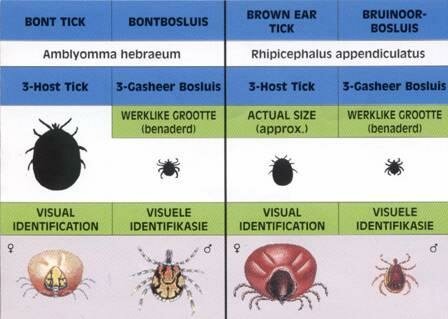
Typical features may include the presence of a black mark where the bite occurred, and fever, severe headache and a rash. The black mark at the site of the tick bite is called an eschar (or a tache noir), and looks like a small ulcer (2-5mm in diameter) with a black centre. It may look something like a spider bite. (I have been there, done that and clearly remember the mother of a headache from 36 years ago).
The eschars can be single or multiple and can sometimes be very difficult to find. The eschar usually appears once the fever appears, as does the headache and malaise (general feeling of ill-health).
Lymph nodes near the eschar may be enlarged. e.g. If you are bitten on the calf, the lymph glands behind your knee and / or in your groin may be painful.
A rash is usually, but not always, a feature of tick bite fever (it is supposedly less likely to occur in someone infected by R. africae), but when it is present, it consists of small red marks on the skin, sometimes raised slightly above the surface. It typically starts on the limbs and spreads to the trunk, and can involve the entire body, including the palms of the hands and soles of the feet.
What is the outcome of ATBF?
African tick bite fever is usually mild, and death and serious complications
are very uncommon.
How is ATBF diagnosed?
Your doctor will examine you and question you about your symptoms and whether you could have had recent exposure to ticks. The typical scenario would be that you had been hiking or camping in a rural or wilderness area, and were therefore in contact with ticks. About a week later, you would have experienced a severe headache, fever and generally felt poorly. You may also have a rash and/or an eschar, and enlarged lymph nodes near the eschar. The presence of the rash and an eschar is a very strong diagnostic sign for tick bite fever.
Because the organism lives inside cells, it is very difficult to culture it in a laboratory, and this isn't routinely offered as a diagnostic test. However, your body makes antibodies (proteins that attack invasive substances or organisms) to the rickettsia, and these can be looked for in the laboratory. These serological tests are the main method of confirming a diagnosis of tick bite fever. However, sometimes the tests only become positive after a couple of weeks, so while they may help to confirm a diagnosis, they are not always immediately helpful early on in the infection. If you have typical symptoms of the infection, and a history of possible exposure to ticks, your doctor may decide to treat you before results of the serological tests are known.
How is ATBF treated?
African tick bite fever is often fairly mild and self-limiting - people may get better on their own without specific treatment. This can take up to two weeks however, and treatment with an antibiotic can shorten the duration of symptoms and reduce the chance of a serious side-effect. The antibiotic doxycycline is the preferred agent for treating tick bite fever. Some people are not able to take doxycycline, in which case chloramphenicol, or sometimes ciprofloxacin, may be used instead. Experience with using ciprofloxacin is more limited than with doxycycline or chloramphenicol.
Can ATBF be prevented?
The easiest may to prevent tick bite fever is to avoid being bitten by ticks. Avoiding rural or wilderness areas where ticks are likely to occur is one way to achieve this, but not a great solution if you enjoy hiking and camping. Other measures are generally common-sense, such as wearing insect repellents and long trousers and sleeves. Look on the insect repellent spray or applicator to see whether they are for the prevention of ticks as well as insects. Bayer make a product called Bayticol® which you spray on your clothes to prevent ticks There is no vaccine against tick bite fever, and taking prophylactic antibiotics (as one does for malaria) has never been shown to be effective or necessary.
If you find a tick on you:
- Use tweezers to firmly grasp the tick at its head or mouth, as close to the skin as possible.
- Pull firmly and steadily on the tick until it lets go of the skin.
- Swab the bite with alcohol or antiseptic.
- Do not use petroleum jelly or light a match to try and remove the tick. I have tried it – it doesn’t work.
Once you have had ATBF you are usually immune to further bites. If your body has not built up enough resistance to the first bite you may get a second bite or more with a reaction described above which will be much less severe depending on your immunity. Please be aware that there are different types of Tick Bite Fever and being infected by one may not necessarily make you immune to another type. Note that the tick also has to be infected with the Rickettsia before it infects you and not all ticks are infected.
When to call the doctor?
Things that should make you suspicious of tick bite fever would be potential exposure to ticks (either by hiking or camping, or you think you've been bitten by a tick imported by your favourite pet!) along with fever, headache, a rash and a black ulcer-like lesion (the eschar). In this sort of rather obvious scenario, it is advisable to see your doctor. Unfortunately, the eschar is not always visible, so the absence of an eschar shouldn't lull you into a false sense of security. Another problem is that the symptoms of fever, headache and a rash are very common (many viral infections, for example, can cause this). In these less obvious situations, the decision of whether or not to consult a doctor depends to some degree on how ill you feel, and what your underlying state of health is (your age, any other health problems, any regular medication etc). As with most illness, some common-sense is required, but if you are in any doubt and you are feeling unwell, it would be best to consult your doctor.
Acknowledgements and references.
- Paper in Health24 written by Dr Andrew Whitelaw, MBBCh (Witwatersarnd), MSc (UCT), FCPath (Micro) (SA) Senior registrar, Department of Microbiology, University of Cape Town and Groote Schuur Hospital.
- Health24 First Aid Removing Ticks http//:health24.com/child/First_aid/833-848,23981.asp
- Raoult D, Fournier PE, Fenollar F, Jensenius M, Prioe T, de Pina JJ, et al. Rickettsia africae, a tick-borne pathogen in travelers to Sub-Saharan Africa. N Engl J Med 2001;344:1504–10.
- Pretorius AM, Birtles RJ. Rickettsia aeschlimannii: a new pathogenic spotted fever group rickettsia, South Africa. Emerg Infect Dis 2002;8:874.